Among people who experience some sort of trauma, what percentage do you think go on to develop post-traumatic stress disorder? A third? A Half? More?
Actually, the answer is 10%. An overestimation of how common it is to develop PTSD after trauma is one of the misconceptions my guest thinks are leading to its overdiagnosis and an underestimation of human resilience.
Dr. Joel Paris is a professor emeritus of psychiatry and the author of Myths of Trauma: Why Adversity Does Not Necessarily Make Us Sick. Today on the show, Joel explains what some of those myths of trauma are, including the idea that it’s trauma itself which causes PTSD. Joel argues that PTSD is instead created when exposure to trauma meets an individual’s susceptibility to it, and he explains what psychological, biological, and even social factors contribute to this susceptibility. We also get into how the methods used to prevent the triggering of trauma can backfire and how the treatment for PTSD will be ineffective if it only focuses on processing an adverse experience.
Resources Related to the Episode
- AoM Podcast #788: The Dangers of “Concept Creep”
- AoM Podcast #555: Dandelion Children vs. Orchid Children
- From Paralysis to Fatigue: A History of Psychosomatic Illness in the Modern Era by Edward Shorter
- AoM Podcast #440: The 3 Great Untruths That Are Setting Up a Generation for Failure
- Jay Belsky’s research on differential sensitivity
- Video demonstration of EMDR
- Radical Acceptance
- Interview with Bruce Wampold as to what makes for a good therapist
- Joel’s other books
Connect With Joel Paris
Listen to the Podcast! (And don’t forget to leave us a review!)
Listen to the episode on a separate page.
Subscribe to the podcast in the media player of your choice.
Listen ad-free on Stitcher Premium; get a free month when you use code “manliness” at checkout.
Podcast Sponsors
Click here to see a full list of our podcast sponsors
Read the Transcript
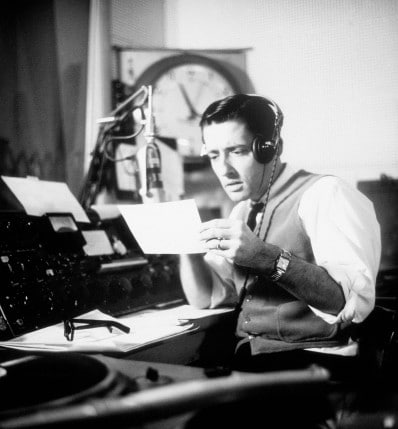
Brett McKay: Brett McKay here and welcome to another edition of the Art of Manliness Podcast. Among people who experience some sort of trauma, what percentage do you think go on to develop post-traumatic stress disorder? A third? A half? Four? Actually, the answer is 10% and overestimation of how common it is to develop PTSD after trauma is one of the misconceptions my guest thinks are leading to its overdiagnosis and an underestimation of human resilience. Dr. Joel Paris is a professor emeritus of psychiatry and the author of Myths of Trauma, why adversity does not necessarily make us sick. Today on the show, Joel explains what some of those myths of trauma are, including the idea that it’s trauma itself which causes PTSD. Joel argues that PTSD is instead created when exposure to trauma meets an individual susceptibility to it. And he explains what psychological, biological, and even social factors contribute to the susceptibility.
We also get into how the methods used to prevent the triggering of trauma can backfire, and how the treatment for PTSD will be ineffective if it only focuses on processing an adverse experience. After the show’s over check out our show notes at aom.is/mythsoftrauma.
Alright. Dr. Joel Paris, welcome to the show.
Joel Paris: Thank you very much for asking me.
Brett McKay: So you are a psychiatrist who specializes in working with individuals with borderline personality disorder. You also do a lot of research on borderline personality disorder, but you’ve recently published a book called The Myths of Trauma, where you take readers on a tour of the history and oft-overlooked research of post-traumatic stress disorder. So why did a researcher and clinician of BPD decide to write a book about PTSD?
Joel Paris: People think that BPD is caused by trauma and that you must have had trauma and that’s the main reason that you have that disorder. And it’s simply not true. It’s an aggravating factor and it’s one of the risk factors of several that lead to BPD, but people have… Some people have wanted to actually redefine BPD as a post-traumatic disorder. And also since I do a less specialized practice consulting for colleagues about various cases, I find that both patients and doctors are all too ready to diagnose anyone with PTSD if they have something bad has happened to them in their lives and this really doesn’t make any sense. It’s an attempt to explain very simply something which is complex, interactive, and multi-dimensional.
Brett McKay: Well, we’ll dig into these ideas more in our conversation, but your book’s called The Myths of Trauma. You’re not saying that trauma itself, this idea is a myth, but there are myths around this idea. So what are the biggest ones? And maybe throughout the conversation we can flesh this out some more.
Joel Paris: Okay. Well, definitely I’m not dismissing trauma. It is important. About 25-30% of the borderline patients that I see have histories like this, but a lot of them don’t. And so the problems are many, first of all, the way the trauma is defined, the DSM is too broad, and then there’s a big discrepancy between exposure to trauma, which is almost universal, somewhere between 75 and 90%, versus the frequency of PTSD after exposure to trauma, which is like 10%. So 90% of people who are exposed to a traumatic event don’t develop PTSD. And PTSD is most clear in a more narrow definition, such as a threat of violence or threat to your life or threat of rape, these are the things which are more likely to cause PTSD, but when people say, “Well, I was emotionally abused in my family,” I mean, that’s a real thing, but it’s not the same thing as the other types of trauma in PTSD. So I think too broad a definition of a traumatic event and a gap between exposure to trauma and actually developing post-traumatic symptoms are some main myths that I discussed in my book.
Brett McKay: Well, let’s talk about this definition of trauma. So you said it’s broad. You’re arguing that it’s too broad. How is it defined clinically and how has that definition changed over the past few decades?
Joel Paris: PTSD got into the diagnostic manual in 1980 with the DSM-III, and that was the first time it appeared. And at that time it had a narrower definition and it got broader over subsequent additions. For example, it’s mentioned that sometimes just hearing about trauma from somebody else without being directly exposed to it or witnessing it, or indirect exposure in the course of your job, that these things could be causes of PTSD makes less sense than as a direct threat against yourself. And I think this is where the beginning of the trouble begins.
Brett McKay: Why did they make it more broad? Okay. So originally it was if you experienced violence, rape, etcetera, that was considered trauma. It’s gotten broader and broader. Like why, why would they do that? What’s the reasoning behind it?
Joel Paris: There’s something called concept creep which a psychologist described a few years ago. When you have a concept in psychology or a construct or a diagnosis, it tends to be increasingly used with time. Now then the second question is, why do the writers of the manual agreed to expand it? Well, they have expanded many of their diagnoses. This is not the only example, that’s a whole other talk in itself, know about the problems with DSM. There may be clinical reasons in that therapists like to make this diagnosis, and there may also be political reasons because people have talked about whether we live in a kind of a post-traumatic society or a traumatic narrative, and that people talk about their traumas and these days I’m hearing from patients they use this language even if they haven’t read the manual. It’s out there and it’s popular because I think people would rather be victims of something else than feel this is something inside them which made them more vulnerable to trauma. One of the main points in my book is that PTSD is not only a result of the exposure, but reflects a vulnerability, a susceptibility to trauma of which there are many, many causes.
Brett McKay: Okay. So one of the arguments you make, one of the myths of trauma is that we’ve broadened the definition too much possibly to make it a useful idea. And this idea of concept creep, we’ve actually had, it was Nick Haslam.
Joel Paris: That’s who I was quoting. Yes.
Brett McKay: Yeah, we had him on the podcast.
Joel Paris: Oh, good.
Brett McKay: That’s episode number 788 for those who wanna listen to that.
Joel Paris: I will look that up.
Brett McKay: But you also, so you mentioned one of the other myths of trauma I think it’s kind of been embedded in our popular culture, psyche, consciousness, whatever you want to call it, is that if someone experiences a traumatic event, I think the assumption is, oh, well that person’s gonna have some sort of PTSD, it’s gonna harm them. But you highlighted numbers like, actually it’s very, very few people who actually experienced a traumatic event go on. So what were those numbers again?
Joel Paris: Well, in general, about 10% of people who are exposed directly to trauma and will develop PTSD later on. And the numbers are somewhat higher for certain things like rape is the worst one, and that gives you a 20% level, although that still means that 80% of people after rape don’t develop PTSD.
Brett McKay: And why do you think this gets overlooked? ‘Cause I think people automatically assume if someone experiences a really severe hardship, they’re gonna have some kind of problem. They need to go get professional help. But you’re showing the numbers actually. I mean, 10%, I mean, it’s terrible for the people who do experience it, but it’s most people, they’re gonna be okay, sounds like.
Joel Paris: Well, yes, this is called resilience and it’s a very central concept in psychology and psychiatry. And resilience is the rule after trauma. And I always say if we weren’t resilient, we would have gone extinct 100,000 years ago. I mean, life was much more traumatic in the past than it is today, in fact. I would refer your listeners to Steven Pinker on that subject. And so I think from an evolutionary point of view, we need to be resilient.
Brett McKay: So I think one of the arguments you make in the book is that this sort of tight coupling between trauma and PTSD that we have in our… Not only amongst the public, but also amongst a lot of clinicians, that it might be increasing the diagnoses of PTSD because someone thinks, “Well, this person had a traumatic event, they automatically have PTSD.” And you’re saying, maybe not.
Joel Paris: Well, I see this all the time because I’m evaluating patients. I do hundreds of consultations a year so I have a lot of experience with this. And if there’s almost anything of this sort in the patient’s past, even just an adverse situation like a dysfunctional family, people write in… After the first diagnosis, they stick in PTSD as a second diagnosis. And some people, and this goes into the latter part of my book where I talk about treatment, some people will prescribe various kinds of what are called trauma focused therapies, even in people who haven’t had the kind of trauma which is most likely to produce PTSD.
Brett McKay: And this is an issue. I’ve heard other clinicians raise concerns about this idea of diagnosing people who probably shouldn’t receive a diagnosis. ‘Cause what it does, people begin to take that identity, “Well, the shrink said I had PTSD, so I must have PTSD,” and they start thinking, “Well, I have PTSD.” But then if they would have gone to another psychiatrist, they probably wouldn’t have gotten that diagnoses and they wouldn’t have been thinking themselves as someone with PTSD.
Joel Paris: Probably not if they’ve seen… Probably less likely if they see somebody like me. It doesn’t even need a shrink to convince people that they have PTSD. People are self-diagnosing all the time. And then they talk about, “Oh, that’s my PTSD acting up,” or, “That’s my ADHD acting up,” and all these diagnoses which are sort of fuzzy and uncertain become a part of your identity. Like you’ve said, it’s a really important point.
Brett McKay: Well, so, okay, so most people don’t get PTSD. Let’s say someone comes to you saying, “Well, I think I got PTSD.” How do you, as a clinician, how are you defining PTSD? If you look at a patient like, yeah, you’ve got something here. We need to help you out. What’s that look like for you?
Joel Paris: Well, I’m following the DSM criteria because they’re most precise. If you look at it, it’s basically exposure to trauma followed by certain characteristic symptoms, most particularly flashbacks, avoiding things that remind you of what happened to you, the so-called triggers, a kind of state of expecting bad things to happen. I mean, there are all kinds of symptoms which are listed in the manual which are required for the diagnosis above and beyond the exposure and people who have PTSD will probably have them and people who don’t will probably not.
Brett McKay: So the research shows that most people who experience a traumatic event, they’re likely not gonna have PTSD, about 10%, 20% in cases of rape. So it sounds like if trauma itself doesn’t cause PTSD, if that’s the case…
Joel Paris: Well, that’s my whole point.
Brett McKay: Yeah. Okay. The trauma itself doesn’t cause PTSD but you say there are other factors that can contribute to it. So what are those other factors?
Joel Paris: Well, first of all, it was noted many years ago, it was a study of Australian firefighters. They were fighting bush fires which is pretty dangerous work. And the nice thing about this study and other similar studies have been conducted since then, but this was was the first study, what they did was they measured some of their personality traits when they started working as firefighters before anything had actually happened to them all, before they’d been in the fire. And they found that people who have what is called very high trait neuroticism, were more likely to develop PTSD after something bad happened in firefighting. So trait neuroticism basically is a central concept in personality theory which describes how easily you’ll get upset and how hard it is to calm down and it could be called being thin-skinned or extremely sensitive. So people who had more of this, were more likely to develop PTSD after exposure. And they’ve done studies like this with policemen and health workers and all kinds of people exposed to trauma. So personality is certainly one of them.
And I should point out here also that trait neuroticism is partially heritable, like all personality traits. There’s about half of it which is you are born with and the other half is due to your life experience so it’s a little bit more complex than that. But it has to do with things about you and how you respond to stressful events and not just the trauma itself.
Brett McKay: Well, so it sounds like some people are just more susceptible. So if they experience a traumatic event and if they’re high on this neuroticism, which as you said, part of it is just genetic, just that’s the luck of the the draw for you. You’re more likely to possibly experience PTSD after that traumatic event.
Joel Paris: Absolutely.
Brett McKay: Okay. Anything else besides the… The personality, any other factors that contribute to a diagnose or more people being susceptible?
Joel Paris: Well, what I proposed in the book is what’s called a biopsychosocial theory, which is bid for many decades, a rather influential concept, and it’s not just for PTSD, it’s for everything in psychiatry. So that… Let me take a step back and say it’s easier for people to think that A causes B and that is one cause, it is one effect, and the world isn’t like that. The world is multivariate. Everything is interactional. Everything that happens to you is complicated. Every response you have to what happens to you in life is equally complicated. And so when we say biopsychosocial, we’re talking about hereditary propensity. And I’ll give you another example of the hereditary propensity while I’m at it.
There was a study of Vietnam vets and we did quite a lot of studies of Vietnam vets. But this one was a twin study of Vietnam vets where they were able to measure the concordance of various mental disorders, including PTSD, and they found for every feature of PTSD, there was a fairly strong heritable component which influenced whether you would get it. So what you’re born with is really quite important. Some people are just born very nervous, and it’s not always a bad thing because cautious people sometimes live longer than risk takers, but it’s still something to… Then there’s a psychological aspect of it and this relates to other aspects of eroticism and other personality traits and also your life experience. So people who’ve had previous mental disorders, particularly those related to anxiety and depression prior to PTSD are more likely to end up with PTSD or even if there’s just a family history. We saw that in the Australian study, that even though there’s just a family history, they’re more likely to develop PTSD. So there are all these psychological factors which affect, which increase the risk.
And then social factors, well, I do talk about this in the book, which is I think the culture of PTSD is part of a larger issue in which people are using psychiatry to validate their sense of victimization in life and people write memoirs about this, and some of them are bestsellers, and sometimes you see these on television. So there’s a whole social structure around it saying it’s not only okay to have PTSD in a way, it’s kind of like almost you should have it because it’s a tough world out there and we need to change the world. So this, some people believe so. But the point about the biopsychosocial model is it’s an interactive model, so one hit won’t give you a mental illness usually. It kind of takes two hits, three hits maybe more, and they all sort of add up and have a cumulative effect and affect each other. So that’s the model they’re proposing and it leads to a different kind of treatment because… I’m sure we’ll get to this. I don’t think that spending all the time discussing the traumatic event itself is always the best idea.
Brett McKay: Okay. So with this biopsychosocial model, it’s complex, it’s non-linear. I think a lot of people, I think particularly the public and just the lay individuals, they think, “Well, if X happened, then Y happened.” They’re very linear thinking and is…
Joel Paris: Well, they’re made that way to think linear.
Brett McKay: Yeah. So I wanna talk more about this social aspect. So we talked about the sort of the biopsycho part of this model. Some people are just born with a propensity to develop mental illnesses, including PTSD if they experience severe adversity in their life. There’s this social model, you call it like the culture of PTSD. You also talked about the culture of trauma. Have there been studies done? I think you particularly see this in the West, in America especially. Have there been studies done across cultures where they look at say a country in Africa or China, for example, where maybe this idea of trauma and PTSD isn’t in the popular psyche? Do they have about the same amount of PTSD diagnoses compared to the United States?
Joel Paris: Well, there are very few systematic or large scale studies of this kind. I mean, it’s expensive and difficult to find out the prevalence of mental disorders in Africa or other developing countries. Nevertheless, I think somewhat partly anecdotally but also based on some of the things I’ve read from anthropologists and cultural psychiatrists, people in other cultures, they have the stress but it comes out differently. For example, fatigue, people just take to their bed and they have no energy. We used to call that in the 19th century psychiatry, neurasthenia. So these kinds of symptoms tend to be more common in developing countries. And I don’t know of anybody who’s gone out to measure PTSD. I’ve been interested in even in the question as to whether or not there’s borderline personalities sort of outside the West. And what I’ve seem to have concluded is that yes, in the large, in very large cities, but no, not in places which haven’t changed in a thousand years.
And there’s something about, I think there’s something about the stresses of modern life, the pace of change. Maybe we could even put a little bit of blame on the internet and social media for spreading all kinds of ideas of how to frame your distress. I mean, the stress, psychological stress is universal, but how it comes out is not as universal. There’s a historian of psychiatry named Edward Shorter, who I think would be interesting for your program, he describes something called the symptom pool and he documented over the last couple of centuries how symptomatic presentations have changed even in the West, and PTSD is probably an example of that but I can’t prove it with hard data.
Brett McKay: You cite some research. Let’s see. Dückers and Brewin, they noted a vulnerability paradox in that PTSD is much more common in highly developed countries than in those afflicted by widespread poverty. And then McNally did a study, he said, he suggested that the paradox can be resolved if PTSD is more frequent in sub-populations within wealthier countries who are more vulnerable. So I guess the idea is that if you grew up in a very affluent life and you don’t have a lot of adversity your standard of what is considered diversity is probably lower than those who grew up in really trying circumstances.
Joel Paris: I think that’s very true. Thank you for the close reading of my book and those references because I did discuss them. Although they’re not based on extensive data, I think those ideas make a lot of sense.
Brett McKay: Okay. So the thing you’re saying again, it’s like, you’re not saying that PTSD doesn’t exist in these, maybe Africa or China or whatever?
Joel Paris: I’m sure it does, but I suspect at a lower, much lower rate.
Brett McKay: Lower rate. Or it might manifest itself differently than here in the United States?
Joel Paris: That’s right, that’s what I’m saying.
Brett McKay: Yeah.
Joel Paris: It may come out of something else which doesn’t look like PTSD, and maybe looks a little bit more like depression or anxiety.
Brett McKay: We’re gonna take a quick break for a word from our sponsors.
And now back to the show. Okay. So yeah this biosocial, psychosocial model shows how complex it is. There’s a lot of factors going on. Just the way you think about PTSD might influence whether you have, will be prone to get PTSD. If you think, well, if I had this traumatic experience, ’cause that’s what everyone’s saying then if you experience a traumatic experience, you think, “Oh, my gosh, I’m gonna get PTSD. I need to go get help.” Some other myths that you highlighted in the book is this idea of repressed memories when it comes to PTSD.
Joel Paris: Yes.
Brett McKay: What’s going on there?
Joel Paris: What’s going on is a fad, well, what I call a malignant fad within psychiatry, it’s not the only one but it was one of the worst. It was most prominent in the 1990s and it was promoted by one psychiatrist who wrote in her book, the usual response to trauma is to forget about it, which is totally untrue because the whole concept of PTSD is that you can’t get it out of your mind, you can’t put it behind you, and the treatment involves, often involves helping people to put it behind them and accept that that happened and then they have to move on. Now, but people are troubled by intense memories of bad things that happened to them and that’s a crucial element of PTSD.
Joel Paris: The idea that trauma is repressed, there’s really almost no evidence for this at all. It was an idea introduced by Sigmund Freud about 130 years ago, and it just has not, it has not been supported by research. But what the fad consists of was hypnotizing people or putting them into very intensive therapies and telling them, you must have been traumatized because look at your symptoms. I mean, I had a patient with borderline personality disorder. She told me her experience as a teenager in the pediatric hospital in Montreal, and she set out with some venom. “They tried to convince me that my father must have molested me and are they wasting my time?” [chuckle] So this idea that you…
There was this book, The Courage to Heal. It sold millions of copies ’cause it appeals to people, it said, “If you have these symptoms you probably were traumatized as a child, and if you can’t remember it that proves that you were traumatized because you repressed it.” It was completely wacko in this respect and yet it appealed to many people. It was only a minority of psychotherapists who embraced or psychiatrists, whoever embraced this idea. But it was out there in the public and there was a small number of people who were promoting it, and I think you’ll still see it. So these ideas of something terrible happened to me, I just have to work to remember it and then process it. This is a very appealing idea for many people.
Brett McKay: Then you also… Maybe you highlight so you’re saying this idea that you, if you experience a traumatic event, you’re likely to repress it. I mean, you go back to the historical record showing Civil War soldiers who… They weren’t diagnosed with PTSD but they basically in their journal entries and their letters they’re, obviously they were traumatized and their problem was they couldn’t forget it. They wanted to get it out of their head, but they’re…
Joel Paris: Exactly, exactly.
Brett McKay: They’re having flashbacks.
Joel Paris: And by the way, soldiers in war, also a majority of them never develop PTSD. But there’s another thing which is particularly relevant for the USA which is that the Veterans Administration offers you free treatments of all kinds if you say you have PTSD and, or if somebody tells you, you have PTSD. It’s an entry into treatments which tend to be not so easily available otherwise.
Brett McKay: So let’s talk about this, this idea you mentioned triggers warnings. You also, you often hear that like I experienced something that triggered my PTSD. There might be something that you hear about people, soldiers particularly, who they might hear some sort of loud noise and it might remind them of an intense memory.
Joel Paris: It is definitely a real phenomenon.
Brett McKay: But then you say there’s some myths around this idea of trigger warnings that have creeped in into our… How we talk about this stuff.
Joel Paris: Well, if you hear a loud noise or even a low flying bird or something like that and you wanna duck, that’s a good example of a trigger that can bring back certain traumatic events. I don’t disagree with that at all. But then it starts becoming like, I was rejected by my partner and that triggered me because of my unhappy childhood. I mean, it starts to spread in Haslam’s concept creep into something which becomes all the pathways to psychopathology can be seen in this model and it’s very tempting.
Brett McKay: Yeah. And it becomes so broad that it, like the idea of triggers becomes useless almost.
Joel Paris: It’s certainly overrated.
Brett McKay: Yeah. And I think that you’ve highlighted research too, this idea. You’re seeing this in college classrooms, this idea of trigger warnings. Oh, we’re gonna discuss something that’s potentially, you know, if you experience this it might trigger you, so if you want to get out, that’s fine. I think you highlight research in the book showing that those actually, they don’t do anything, like in…
Joel Paris: No. Well, in fact, this is the whole probable, and the whole culture in the university and the trigger warnings. I went to a lecture at my university from an expert in a rather controversial field which is gender identity. And at the beginning of the… And before I was being introduced the moderator announced that, “If you get too upset by anything this person says, we have people in the back ready to talk to you.” I think that Jonathan Haynes and others, Christakis, people, academics have talked about this as something which is really undermining free speech and diversity because somebody’s going to be triggered by it. And it’s kind of like a weird idea that young people could be so easily triggered that they have to be in the words of these academics coddled, rather than be in an environment where you can pose difficult questions and look for answers.
Brett McKay: Yeah. You highlight research from Bellet, he has had this to say, I thought it was really interesting. He says, “Trigger warnings may raise awareness of the difficulties of people suffering PTSD. However, they may also create the impression that the experience of trauma always renders survivors emotionally incapacitated.” And we talked about this. “In reality, most trauma survivors are resilient and show few symptoms of PTSD after initial period of adjustment. The perception of trauma survivors as dysregulated victims may contribute to negative stigma concerning the very individuals trigger warnings are intended to protect.”
Joel Paris: And it works somewhat against the idea of confidence mastery, getting a life, having an identity, feeling realistically optimistic about one’s options. All these things is infantilizing.
Brett McKay: Yeah. So we talked about what can cause people to get PTSD and some of the myths around that. Again, you highlight research, most people aren’t affected about 90 to 80%. If they experience a traumatic event, they’re gonna be okay. But then you also highlight research that some people actually become more emotionally and mentally robust after a traumatic event. What’s going on there?
Joel Paris: That’s called post-traumatic growth. And the people like to quote Nietzsche who said, “What doesn’t kill me makes me stronger.” But in terms of science, there’s a lot of research on resilience and people who’ve been through terrible things, you know, most of them will cope. There’s a whole enormous literature and psychology about resilience and it’s probably related to what’s been called positive psychology, whereas I think this trauma focus could be called negative psychology.
Brett McKay: On this idea of post-traumatic growth syndrome, are there some people who just have more of a propensity for that than others?
Joel Paris: Well, again, the highly neurotic people by nature are probably going to have more difficulty getting out of their traumas than people who could just… So there are some people who just bad things happen to them and they just shake them off and move on. They’re very low in neuroticism. So I think this is a very important factor in terms of how much people tend to get better without treatment and how much better they’ll get within treatment.
Brett McKay: And this idea that, okay, some people will experience growth, some people will have a hard time after they experience traumatic events. Others reminds me of a podcast we did a couple years ago about children, and there’s this idea that some children are born orchids and some are born dandelions.
Joel Paris: I love that, I love that.
Brett McKay: Yeah. The dandelion kids, like you could put them in any situation and they’ll be okay ’cause they’re like weeds or they’re like dandelions or robust. But then some kids, because of genetics and whatever, they’re more like orchids and they require a more… A better environment, they can’t handle a lot of stress. And I think it’s a interesting thing to keep in mind as you’re thinking about this stuff.
Joel Paris: Well, Jay Belsky has written about this too, he’s a well known psychologist, and he just calls a differential sensitivity to the environment and he suggests that actually these people who are easily upset are also more permeable to good things that happen to them. So they may actually do better than the average person if they’re in a very positive environment, but they do much worse if they’re in a negative one.
Brett McKay: So let’s talk about treatment. What are some of the biggest myths about the treatment of PTSD and other trauma related disorders?
Joel Paris: Well, I think the biggest one is that the treatment should only be about processing the trauma and this is the problem with several of the methods that I described in my book. I’m somewhat negative about EMDR, this eye movement thing where if you have ever seen a video of this being done, that it reminds me of Mesmer from the 18th century with a wand, waving and then the eye movements which has not been shown to make any difference. EMDR is no better than most standard therapies which are being offered to these patients. But it’s trendy, it was marketed very cleverly by this woman, Shapiro, who developed it, and some people come in asking for it and so… But in fact, I think we could live without it. There are variations of cognitive behavior therapy which have a traumatic focus, which make more sense. You do have to talk about the trauma. I’m not suggesting in any way we should avoid talking about it and it’s always worth going into it.
The question is whether or not healing happens because you’ve processed the trauma or whether healing happens because something larger like your sense of self-identity, direction, your relationship, your career, you’ve got things to protect you and guide you through recovery, which can be supported and reinforced in psychotherapy. And I think those broader aspects of therapy, which have sometimes been called the common factors in therapy, the ones that make you feel that somebody has understood you and you can get better and you don’t have to give in to all of these things. This is what works for most people in therapy. And not seeing that broader picture may be a negative in terms of what we offer for patients who do have PTSD.
Brett McKay: Okay, so what you’re saying is the bottom line therapy for PTSD is as long as you’re with a therapist who you feel like you’re understood, you have a good relationship with them, they give you a sense of hope that you can get over this and move on with your life and be robust, that’s probably the more important thing compared to the specific therapy you use.
Joel Paris: The research totally supports that. There’s a guy in Wisconsin called Bruce Wampold who’s been writing about this for decades, and the evidence overwhelmingly shows that techniques in therapy are much less important than the relationship. And that the ability to get people better is as much a talent, a personal talent to the person who provides a treatment as it is anything nuts and bolts specific that they do.
Brett McKay: And I think this could apply to other mental health things that you might, if you want [0:35:18.3] ____.
Joel Paris: Generally, it’s generally true in all the non-psychotic mental health conditions, anxiety, depression, personality disorders. We certainly do a bit of trauma work when we treat our patients with borderline personality disorder in the clinics that I run, but it’s part of a larger frame and we’re very influenced by Marsha Linehan’s DBT, which emphasizes something called a radical acceptance, which goes back to the stoics and philosophy in some ways. And that you encourage people to say whatever’s happened to you in the past, it’s in the past, the future is in your hands, you can make it better. I’ll coach you to get there, but you don’t have to be hobbled by the past. But before you… But in order to do that you have to accept that it’s happened and you can’t change it and… But not see that yourself is doomed to be marked by it for the rest of your life. So this is a… This crucial concept in dialectical behavior therapy of radical acceptance we use it a lot and I think it’s just as relevant to trauma as some of the other more trauma specific things that have been described.
Brett McKay: And one of the arguments you make and this is bolstered by other researchers you cite, is that the focusing on treatment where you just talk about the trauma over and over again, it’s not helpful and actually can backfire because it just ingrains in the person’s head that, “Well, I can’t do anything about this. This happened to me and there’s no hope and I just kinda had to muddle along through life.”
Joel Paris: They had these trauma counselors who were some at one point were being flown into various disasters to talk to people right away and they found that that definitely made people worse because they haven’t even gotten past the stage of being so-called shock yet. And I think you have to respect trauma, validate the person’s right to be upset about it but not indicate that somehow by going over and over the same thing, they can get better without doing something in their present life to make a difference.
Brett McKay: Yeah. I thought it was interesting that the studies about the trauma counselors, I remember hearing about that 10, 15 years ago when there would be a natural disaster or even at 9/11, they would fly in these trauma counselors so they could just talk to these people right away. And I think it was well intended. They thought, “Well, these people had a hard time. If we just talk to them right away, maybe you can diminish the amount of PTSD they might experience.” But it actually backfired because like, I guess the body or in the mind, they have… We have a natural way of processing traumatic events and if we, I don’t know, talk about it too much, it might disrupt that natural process.
Joel Paris: I totally agree with you.
Brett McKay: Yeah. And I think you still see it nowadays. I’ve seen it at schools where a teacher might die and they’ll have grief counselors right away. And it reminded me of the trauma counselors. I don’t… Maybe it’s helpful, maybe some students need that, but maybe, maybe not, maybe there’s just kids who just need to kind of get together and talk about it on their own and they’ll, I mean, maybe they’ll figure it out.
Joel Paris: Absolutely. And I think and of course that also relates to the situation of trigger warnings in universities, in classrooms is the same issue. They don’t know, the counselors, they hear something which is upsetting, you have to learn about things which are upsetting, that’s part of education.
Brett McKay: Okay. So when you treat someone with borderline personality disorder or PTSD, you’re gonna talk about the trauma, yet people need to feel they’re heard and understood, but then I guess you’re saying the better thing to do instead of focusing on that, continuing to focus on that, is to talk about what are some things I can do now to make things better? Like restore agency in people’s lives.
Joel Paris: Agency is a lovely word, and I totally agree with what you’ve just said. That’s my position.
Brett McKay: Okay. Well, this has been a great conversation. Is there any place people can go to learn more about the book and your work?
Joel Paris: Well, I am on the Author Center at Amazon. [laughter] I’ve written 25 books mostly on personality disorders but also on [0:39:29.0] ____ in general. This one is published by Oxford University Press, it came out in October, it’s in a paperback it’s not that expensive. So if people want to look for it, I think Amazon is the easiest place to go.
Brett McKay: Fantastic. Well, Joel Paris, thanks for your time, it’s been a pleasure.
Joel Paris: Thank you.
Brett McKay: My guest here is Dr. Joel Paris, he’s the author of the book the Myths of Trauma. It’s available on amazon.com. Check out our show notes at aom.is/mythsoftrauma where you’ll find links to resources, where you can delve deeper into this topic.
Well, that wraps up another edition of the AOM podcast. Make sure to check out our website at artofmanliness.com where you find our podcast archives as well as thousands of articles written over the years about pretty much anything you can think of. And if you’d like to enjoy ad-free episodes of The AOM podcast, you can do so on Stitcher Premium. Head over to stitcherpremium.com, sign up, use code MANLINESS to checkout for a free month trial. Once you’re signed up, download the Stitcher App on Android, iOS and you start enjoying ad-free episodes of the AOM podcast. And if you haven’t done so already, I’d appreciate it if you’d take one minute to give us a review on Apple Podcast or Spotify, it helps out a lot. If you’ve done that already, thank you. Please consider sharing the show with a friend or family member who you think will get something out of it. As always thank you for the continued support. Until next time, this is Brett McKay, reminding you to not only listen to podcast, but put what you’ve heard into action.